7 Resources for Nurse Practitioners to Decode Primary Care Billing and Coding
From insurance reimbursement and billing to coding and audits, these responsibilities can leave any healthcare provider with goosebumps – especially those who work in or own their own private practice. The most stressful part, in relation to insurance reimbursement, is that most healthcare providers like nurse practitioners are not formally trained in billing and coding and work in a clinical setting or facility with no certified billing and coding specialists. Luckily, there are a wide variety of resources available to help decode this unfamiliar territory.
Coding Basics
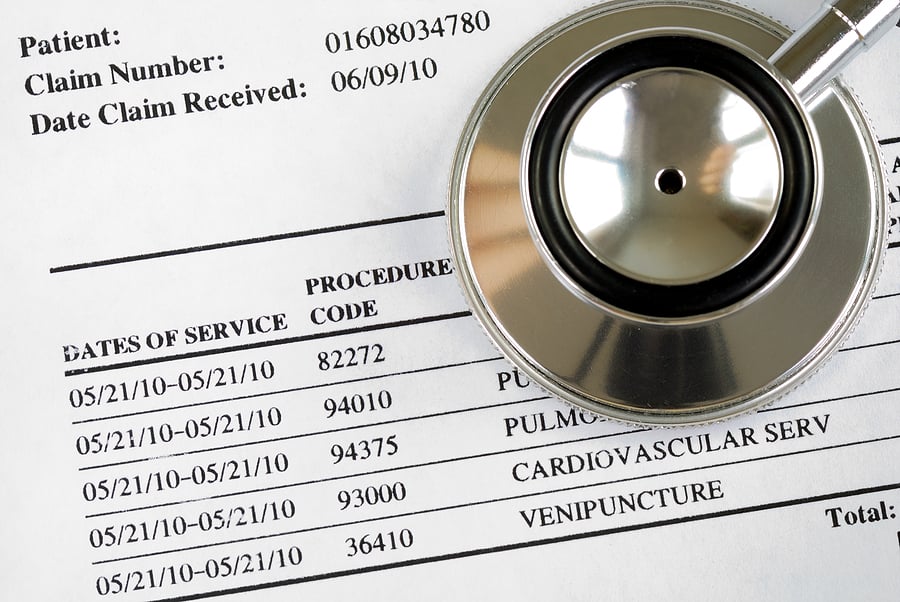
Accurate coding is critical for insurance reimbursement, succinct documentation, and identifying clinical care gaps. The Healthcare Common Procedure Coding System (HCPCS) codes and International Classification of Diseases, 10th Revision (ICD-10) codes serve as the building blocks of medical coding.
- HCPCS Level I codes: These codes are used to describe medical, surgical, diagnostic, and other types of medical services. In addition, there are modifiers that help identify alterations to HCPCS codes.
- Category I: Common procedures
- Category II: Performance measurements
- Category III: Emerging technologies
- HCPCS Level II codes: These codes are used to describe products, supplies, and services provided during an encounter.
- ICD-10 codes: These codes are used to describe the reason for a patient encounter or outline a patient's characteristics, and are essential for identifying common diagnoses in a medical practice. They notify the insurance payer of the medical necessity of the visit.
Evaluation/Management Coding
Evaluation/Management (E/M) coding is the core of healthcare billing and insurance reimbursement. Understanding E/M coding can help maximize the insurance reimbursement of a practice and reduce stress levels during audits. These codes are based on several factors:
- The patient's history
- The patient's physical exam
- The provider's medical decision making
- The appointment time, specifically if the provider spent 50% of the visit coordinating care or counseling
There are different levels for the aforementioned factors, which decipher which E/M code to use.
- History
- Problem-focused
- Expanded problem-focused
- Detailed
- Comprehensive
- Physical Exam
- Problem-focused
- Expanded problem-focused
- Detailed
- Comprehensive
- Medical Decision Making
- Straightforward
- Low complexity
- Moderate complexity
- High complexity
The level of complexity related to medical decision making depends on the number of diagnoses and management options, the complexity of the patient data that was reviewed, and the risk of complications or morbidity/mortality.
Transition of Care Billing and Coding
Transition of care visits are an efficient way to support the continuity of care after a patient is discharged from a skilled nursing facility/nursing facility, long-term acute care hospital, rehabilitation hospital, acute care hospital, or observation stay in a hospital. A transition of care visit can only be billed one time per patient in a 30-day timeframe, and can be billed for both new and established patients at a particular clinic.
Transition of care visits can be billed using two different codes.
- 99495-This code can only be used if the patient has been contacted within two business days of their discharge, the medical decision making is of moderate complexity, and there is an in-person clinic visit within 14 days of the discharge.
- 99496- This code is used if the patient has been contacted within two business days of their discharge, the medical decision making is of high complexity, and there is an in-person clinic visit within seven days of the discharge.
Medicare Wellness Coding and Billing
Medicare wellness exams go beyond a typical annual adult wellness examination. In addition to focusing on a patient's wellness, these exams involve a thorough screening centered around disease prevention. The exam also takes a more comprehensive look at the patient's vital signs, medical/family history, and health risk assessments including their emotional and psychological well-being to develop a personalized prevention plan. Many types of healthcare providers can complete these wellness exams, including:
- Physicians
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Registered dietitians
- A team of medical professionals with an overseeing physician
RELATED: Complete Guide to the Adult-Gerontology Nurse Practitioner Specialty
Pediatric Coding and Billing
Accurate coding for the pediatric population is similar to the process for the adult population with several additional considerations including behavior screenings, developmental screenings, and vaccine administration. Another complication is that not all of these screenings and vaccines are completed at every age. Each well child examination typically has different screenings and different vaccine administrations or they may not have any vaccines at all. That's why it is important to follow the recommendations of Bright Futures, which establishes guidelines that insurances follow.
RELATED: Complete Guide to the Pediatric Nurse Practitioner Specialty
Initially, the billing and coding world can be daunting and confusing. Luckily, there are a variety of resources available to help providers make sense of this information. In addition to online resources, there are several textbooks and conferences that can strengthen a provider's knowledge of accurate billing and coding. Accessing the right resources can help providers boost their understanding, which leads to more efficient documentation, increased reimbursement, and decreased stress during chart audits.
- 4 Essential Projects to Improve Primary Care Office Flow for Nurse Practitioners - October 31, 2020
- Keeping Your Sanity: How to Prevent Nurse Practitioner Burnout - October 6, 2020
- How NPs Can Tackle Difficult Conversations with Patients and Families - September 30, 2020
Related Articles
- 7 Pros and Cons of Becoming a Family Nurse Practitioner (FNP)
- Dear NP Student, From a New Grad NP: Study Tips
- Student Loan Forgiveness: 4 Options for Nurse Practitioners
- A 7 Step Health Policy Toolkit to Flex Your Political Muscle as a Nurse Practitioner
- Is the DNP Worth It? Four Reasons Why Nurse Practitioners May Feel Cautious
- 5 Unexpected Perks of Joining a Professional Nurse Practitioner Organization
